A novel blood type, Junior negative, has been identified in a woman from Guadeloupe, marking a significant discovery in hematology and potentially impacting transfusion medicine.
French scientists have identified an extremely rare blood type, Junior negative, in a patient from Guadeloupe, a French territory in the Caribbean. This discovery, reported by the French National Institute of Blood Transfusion (INTS), highlights the complexities of blood typing and the potential risks associated with blood transfusions, especially for individuals with rare blood types. The finding underscores the importance of comprehensive blood screening and personalized transfusion strategies to ensure patient safety. This newly recognized blood type adds another layer of intricacy to the already complex world of blood groups and their compatibility.
The woman’s case came to light after she experienced complications related to an existing health condition, requiring repeated blood transfusions. Standard blood typing methods failed to find compatible blood for her, prompting further investigation. According to the INTS, the woman has a deletion in the ABCB6 gene, which is responsible for producing the Junior blood group antigen. This genetic anomaly means her red blood cells lack the Junior antigen, making her Junior negative.
“This is only the second known case worldwide of a complete deficiency in the Junior blood group system,” stated Dr. Stephan Rouger, head of the INTS laboratory that made the discovery. The first such case was identified in 2011 in a patient of Iranian descent. The rarity of this blood type presents significant challenges in ensuring compatible blood is available for this patient and others who may share this extremely rare characteristic.
The discovery has important implications for transfusion medicine and prenatal care. Individuals with rare blood types can develop antibodies if exposed to blood containing the antigens they lack. These antibodies can cause transfusion reactions if they receive incompatible blood in the future. In pregnant women, these antibodies can cross the placenta and attack the red blood cells of the fetus, leading to hemolytic disease of the fetus and newborn (HDFN).
“The discovery underscores the importance of considering rare blood groups in transfusion medicine,” emphasized Dr. Rouger. “It also highlights the need for more comprehensive screening of blood donors to identify individuals with rare blood types.” The French National Institute of Blood Transfusion is working to develop strategies to better manage patients with rare blood types, including creating a national registry of individuals with rare blood groups and developing specialized blood products for these patients.
The identification of this new case of Junior negative blood is a critical step forward in understanding the complexities of blood groups and improving the safety of blood transfusions. The researchers hope that this discovery will lead to better screening methods and more personalized transfusion strategies for patients with rare blood types, preventing potentially life-threatening complications. The case also brings attention to the need for greater diversity in blood donation to ensure that rare blood types are adequately represented in blood banks. This ensures that individuals with these rare blood types have access to compatible blood when they need it most.
Understanding Blood Groups and the Junior System
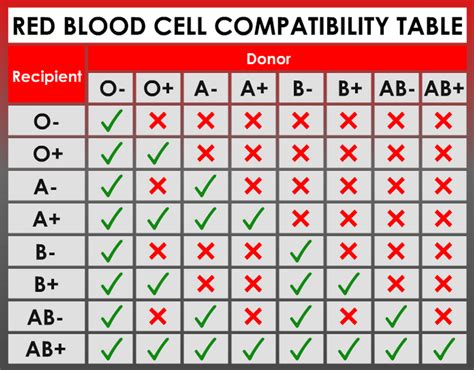
Blood groups are classified based on the presence or absence of specific antigens on the surface of red blood cells. These antigens are inherited and determined by an individual’s genes. The most well-known blood group system is the ABO system, which classifies blood into four main types: A, B, AB, and O. Another important blood group system is the Rh system, which determines whether a person is Rh-positive or Rh-negative.
In addition to these major blood group systems, there are many other less common blood groups, each with its own set of antigens. The Junior blood group system is one such system, characterized by the presence or absence of the Junior antigen, also known as ABCB6. The ABCB6 protein is a transmembrane transporter that plays a role in the transport of porphyrins, which are essential components of hemoglobin.
Individuals who have the Junior antigen are considered Junior positive, while those who lack the antigen are Junior negative. The Junior negative blood type is relatively rare, but it is more common in certain populations. For example, it is estimated that approximately 50,000 to 75,000 Europeans are Junior negative. However, among individuals of Japanese descent, the prevalence is much higher, estimated at approximately 1 in 1,000.
The discovery of the Junior blood group system dates back to 1995 when scientists identified the ABCB6 gene as the gene responsible for the Junior antigen. Since then, researchers have been studying the role of the Junior antigen in red blood cell function and its implications for transfusion medicine.
Clinical Implications of Junior Negative Blood
The primary clinical concern associated with Junior negative blood is the risk of alloimmunization. This occurs when a Junior negative individual is exposed to Junior positive blood through transfusion or pregnancy. The immune system recognizes the Junior antigen as foreign and produces antibodies against it. These antibodies can then cause problems in future transfusions or pregnancies.
In transfusion medicine, alloimmunization can lead to transfusion reactions. If a Junior negative patient who has developed anti-Junior antibodies receives Junior positive blood, the antibodies will attack the transfused red blood cells, causing them to be destroyed. This can result in a range of symptoms, from mild fever and chills to severe complications such as kidney failure and even death.
In pregnant women, anti-Junior antibodies can cross the placenta and attack the red blood cells of the fetus if the fetus is Junior positive. This can lead to hemolytic disease of the fetus and newborn (HDFN), a condition in which the fetus’s red blood cells are destroyed, leading to anemia, jaundice, and other complications. In severe cases, HDFN can be life-threatening.
Challenges in Managing Junior Negative Patients
Managing Junior negative patients presents several challenges for healthcare providers. One of the main challenges is the difficulty in finding compatible blood for transfusion. Because Junior negative blood is relatively rare, it can be difficult to locate donors who have this blood type. This can be especially problematic in emergency situations when a patient needs a blood transfusion quickly.
Another challenge is the potential for alloimmunization. Even if a Junior negative patient receives compatible blood for their first transfusion, they can still develop anti-Junior antibodies if they are exposed to Junior positive blood in the future. This means that healthcare providers need to be vigilant in monitoring Junior negative patients for the development of antibodies and taking steps to prevent alloimmunization.
Strategies for Managing Junior Negative Patients
Several strategies can be used to manage Junior negative patients and minimize the risks associated with this rare blood type. One important strategy is to perform thorough blood typing on all patients who may require blood transfusions. This includes testing for the Junior antigen and other less common blood group antigens.
Another important strategy is to use leukoreduced blood for transfusions. Leukoreduction is a process that removes white blood cells from donated blood. White blood cells can trigger alloimmunization, so using leukoreduced blood can help to reduce the risk of patients developing antibodies against the Junior antigen.
For pregnant women who are Junior negative, it is important to monitor them closely for the development of anti-Junior antibodies. If antibodies are detected, the fetus should be monitored for signs of HDFN. In some cases, intrauterine transfusions may be necessary to treat the fetus.
The Importance of Rare Blood Donor Registries
Given the challenges in finding compatible blood for patients with rare blood types, rare blood donor registries play a crucial role in transfusion medicine. These registries maintain a database of individuals with rare blood types who are willing to donate blood when needed. When a patient with a rare blood type requires a transfusion, healthcare providers can consult the registry to find a compatible donor.
Rare blood donor registries are typically maintained by blood banks or transfusion centers. These organizations actively recruit individuals with rare blood types to join the registry. They also work to raise awareness of the importance of rare blood donation among the general public.
In the case of the Junior negative blood type, several rare blood donor registries exist around the world. These registries work to connect Junior negative patients with compatible donors, ensuring that they have access to the blood they need. The French National Institute of Blood Transfusion is actively developing a national registry to improve access for patients like the woman in Guadeloupe.
The Global Impact of Rare Blood Types
The discovery of rare blood types like Junior negative is not limited to specific geographic regions. While the Guadeloupe woman’s case highlights a particular instance, the implications resonate globally. Different populations exhibit varying frequencies of rare blood types due to genetic diversity and historical migration patterns.
For example, the Diego (Di(a)) positive blood type is rare in most populations but is relatively common among South American Indigenous people. Similarly, the Duffy-negative blood type, which provides resistance to certain types of malaria, is prevalent in populations of African descent.
Understanding the distribution of rare blood types across different populations is crucial for several reasons:
-
Tailoring Transfusion Strategies: Healthcare providers can tailor transfusion strategies to match the specific needs of patients from different ethnic backgrounds. This includes screening donors for rare antigens that are more common in certain populations.
-
Preventing Hemolytic Disease of the Fetus and Newborn: Identifying pregnant women with rare blood types and monitoring them for the development of antibodies can help prevent HDFN.
-
Optimizing Blood Bank Inventories: Blood banks can optimize their inventories by stocking blood products that are compatible with the most common rare blood types in their service area.
-
Facilitating International Blood Exchange: Collaboration among blood banks in different countries can facilitate the exchange of rare blood products when needed.
The Future of Blood Typing and Transfusion Medicine
The field of blood typing and transfusion medicine is constantly evolving. New technologies and techniques are being developed to improve the accuracy of blood typing, enhance the safety of blood transfusions, and expand the availability of blood products.
One promising development is the use of molecular blood typing. This technique uses DNA analysis to identify an individual’s blood type. Molecular blood typing is more accurate than traditional serological methods and can be used to identify rare blood types that are difficult to detect using conventional methods.
Another area of active research is the development of artificial blood. Artificial blood substitutes are designed to carry oxygen and deliver it to tissues in the body. These substitutes could potentially overcome the limitations of donated blood, such as the shortage of rare blood types and the risk of transfusion-transmitted infections.
Furthermore, advancements in precision medicine are paving the way for personalized transfusion strategies. By considering an individual’s genetic makeup, medical history, and specific clinical needs, healthcare providers can tailor transfusion protocols to minimize the risk of complications and maximize the benefits of transfusion.
The Importance of Diversity in Blood Donation
The discovery of the Junior negative blood type in the Guadeloupe woman underscores the critical need for diversity in blood donation. Rare blood types are more common in certain ethnic groups, and a lack of diversity in the donor pool can make it difficult to find compatible blood for patients from those groups.
Blood banks around the world are actively working to recruit more donors from diverse backgrounds. These efforts include outreach programs, educational campaigns, and partnerships with community organizations. By increasing the diversity of the donor pool, blood banks can ensure that all patients have access to the blood they need, regardless of their ethnicity or blood type.
The case also highlights the need for increased awareness of rare blood types among healthcare professionals. By educating doctors, nurses, and other healthcare providers about the complexities of blood typing and the importance of considering rare blood types, we can improve the care of patients with these unique characteristics.
Conclusion
The identification of the Junior negative blood type in the Guadeloupe woman is a significant discovery that has important implications for transfusion medicine and prenatal care. This case underscores the complexity of blood groups and the potential risks associated with blood transfusions, especially for individuals with rare blood types. It also highlights the need for more comprehensive screening of blood donors and the development of personalized transfusion strategies.
The French National Institute of Blood Transfusion and other organizations around the world are working to address the challenges posed by rare blood types. By improving blood typing methods, developing rare blood donor registries, and promoting diversity in blood donation, we can ensure that all patients have access to the blood they need, regardless of their blood type.
The ongoing research and advancements in blood typing and transfusion medicine offer hope for a future where blood transfusions are safer and more effective for all patients. By embracing innovation and fostering collaboration, we can continue to improve the lives of individuals with rare blood types and those who rely on blood transfusions for their health and well-being.
Frequently Asked Questions (FAQs)
- What is the Junior negative blood type?
The Junior negative blood type is a rare blood type characterized by the absence of the Junior antigen (ABCB6) on red blood cells. Individuals with this blood type can develop antibodies if exposed to Junior positive blood, potentially leading to transfusion reactions or hemolytic disease of the fetus and newborn (HDFN) during pregnancy. “This is only the second known case worldwide of a complete deficiency in the Junior blood group system,” according to Dr. Stephan Rouger, head of the INTS laboratory.
- How rare is the Junior negative blood type?
The Junior negative blood type is considered very rare. While its prevalence varies depending on the population, it’s significantly less common than more well-known blood types like A, B, AB, and O. In Europeans, it’s estimated that approximately 50,000 to 75,000 individuals are Junior negative, whereas among individuals of Japanese descent, the prevalence is around 1 in 1,000. This rarity poses challenges in finding compatible blood for transfusion.
- What are the risks associated with Junior negative blood?
The main risks associated with Junior negative blood are alloimmunization and subsequent transfusion reactions. If a Junior negative person receives Junior positive blood through a transfusion or pregnancy, their body can develop antibodies against the Junior antigen. These antibodies can then attack transfused red blood cells or fetal red blood cells if the fetus is Junior positive, potentially causing serious health complications.
- How is the Junior negative blood type managed?
Management of Junior negative individuals involves careful blood typing to identify their rare blood type, using leukoreduced blood for transfusions to minimize the risk of alloimmunization, and monitoring pregnant women for the development of anti-Junior antibodies. Rare blood donor registries also play a vital role in connecting patients with compatible donors. “The discovery underscores the importance of considering rare blood groups in transfusion medicine,” stated Dr. Rouger, highlighting the need for comprehensive screening.
- What is the significance of this discovery in Guadeloupe?
The discovery of the Junior negative blood type in a woman from Guadeloupe is significant because it highlights the importance of considering rare blood types in transfusion medicine. This case underscores the need for more comprehensive screening of blood donors, particularly in diverse populations, to ensure that individuals with rare blood types receive compatible transfusions. The finding also emphasizes the role of research in advancing our understanding of blood groups and improving patient care. It reinforces the urgency for developing national registries and specialized blood products for patients with rare blood types.









