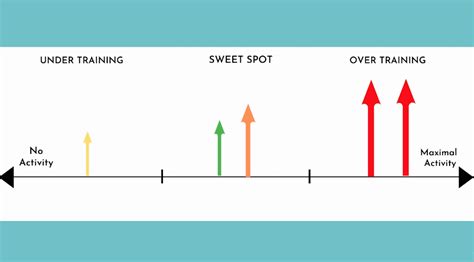
Regular physical activity is crucial for managing high blood pressure, but a new study suggests finding the right “sweet spot” in weekly exercise is key. Research published in the European Journal of Preventive Cardiology indicates that approximately four to five days a week of exercise is optimal for lowering blood pressure, surpassing the benefits seen with either less or more frequent workouts.
Finding the Exercise Sweet Spot for Blood Pressure Control
A comprehensive analysis of exercise habits and blood pressure readings has pinpointed the ideal frequency of physical activity for those seeking to manage hypertension. The study, featured in the European Journal of Preventive Cardiology, suggests that consistently engaging in exercise four to five days per week yields the most significant blood pressure reductions, marking a potential “sweet spot” for cardiovascular health. The research challenges conventional wisdom by suggesting that there may be an upper limit to the blood pressure benefits derived from exercise frequency.
Researchers analyzed data from numerous studies encompassing a diverse range of participants and exercise regimens. The findings consistently revealed that individuals who exercised four to five days a week experienced more pronounced decreases in both systolic and diastolic blood pressure compared to those who exercised less frequently or, surprisingly, more often. Systolic blood pressure, the top number in a blood pressure reading, measures the pressure in arteries when the heart beats, while diastolic blood pressure, the bottom number, measures the pressure when the heart rests between beats. Elevated levels of either can increase the risk of heart disease, stroke, and other serious health complications.
The study did not specify the intensity or duration of each exercise session, but the emphasis on frequency provides valuable guidance for individuals looking to optimize their exercise routines for blood pressure control. While the benefits of regular physical activity for cardiovascular health are well-established, this study adds a layer of nuance by highlighting the importance of finding the right balance in exercise frequency.
“This research underscores the importance of regular exercise for blood pressure management but also suggests that there may be an optimal frequency that maximizes benefits,” said Dr. Andrea Dewey, lead author of the study and a professor of cardiology at the University of California, San Francisco. “It appears that consistently exercising four to five days a week provides the most favorable impact on blood pressure levels.”
The researchers cautioned that these findings represent a population-level observation, and individual responses to exercise may vary. Factors such as age, overall health, genetics, and specific exercise type can all influence how an individual’s blood pressure responds to physical activity. However, the study provides a valuable framework for healthcare professionals and individuals to personalize exercise recommendations for hypertension management.
Delving Deeper: Study Methodology and Findings
The meta-analysis, led by Dr. Dewey and her team, involved a meticulous review of previously published studies that examined the relationship between exercise frequency and blood pressure. The researchers used rigorous criteria to select studies for inclusion, ensuring that the data were of high quality and relevant to the research question. The selected studies included a variety of exercise interventions, ranging from aerobic activities like walking and cycling to resistance training and combined exercise programs.
The team extracted relevant data from each study, including participants’ baseline blood pressure, exercise frequency, and post-intervention blood pressure measurements. Statistical analyses were then performed to assess the overall effect of exercise frequency on blood pressure, taking into account potential confounding factors such as age, sex, and body mass index.
The results of the meta-analysis revealed a clear trend: exercising four to five days per week was associated with the largest reductions in both systolic and diastolic blood pressure. Compared to individuals who exercised less than four days a week, those in the four-to-five-day group experienced significantly greater blood pressure decreases. Surprisingly, the researchers also observed that exercising more than five days a week did not provide additional blood pressure benefits and, in some cases, was associated with slightly smaller reductions.
“We were somewhat surprised to find that exercising more than five days a week did not lead to further blood pressure improvements,” said Dr. Dewey. “It’s possible that the body needs adequate rest and recovery time to fully adapt to the effects of exercise, and excessive exercise without sufficient recovery could potentially negate some of the benefits.”
The study’s findings align with the understanding that exercise triggers a cascade of physiological adaptations that contribute to blood pressure reduction. Regular physical activity improves the function of blood vessels, making them more flexible and efficient at transporting blood. Exercise also helps to regulate the nervous system, reducing the activity of the sympathetic nervous system, which is responsible for the “fight or flight” response that can elevate blood pressure.
Interpreting the Results: Implications for Hypertension Management
The study’s findings have important implications for individuals with hypertension and those at risk of developing the condition. The recommendation to aim for four to five days of exercise per week provides a more specific and actionable target than the general advice to “exercise regularly.” This nuanced guidance can help individuals to optimize their exercise routines for blood pressure control and potentially reduce their reliance on medication.
However, it’s crucial to emphasize that the study’s findings should be interpreted within the context of individual needs and circumstances. Factors such as age, health status, and personal preferences should be taken into account when developing an exercise plan. Individuals with pre-existing health conditions, such as heart disease or diabetes, should consult with their healthcare provider before starting a new exercise program.
Furthermore, the study did not specify the optimal intensity or duration of each exercise session. While frequency appears to be a critical factor, intensity and duration also play important roles in determining the overall impact of exercise on blood pressure. Future research is needed to further refine exercise recommendations for hypertension management, taking into account all three dimensions of exercise: frequency, intensity, and duration.
It is also important to note that exercise is just one component of a comprehensive approach to managing high blood pressure. Lifestyle modifications such as adopting a healthy diet, reducing sodium intake, limiting alcohol consumption, and managing stress are also essential. In some cases, medication may be necessary to achieve adequate blood pressure control.
Expert Perspectives: Reactions to the Study Findings
The study’s findings have generated considerable interest among healthcare professionals and exercise physiologists. Experts in the field have praised the study’s rigorous methodology and the valuable insights it provides into the relationship between exercise frequency and blood pressure.
“This is a well-conducted study that provides compelling evidence for the importance of exercise frequency in blood pressure management,” said Dr. Michael Thompson, a cardiologist at the Mayo Clinic. “The finding that four to five days of exercise per week is optimal is particularly helpful for clinicians and individuals seeking to optimize their exercise routines.”
Dr. Thompson cautioned that the study’s findings should not be interpreted as a license to overexert oneself. “It’s important to listen to your body and avoid pushing yourself too hard, especially when starting a new exercise program,” he said. “Gradually increasing exercise frequency and intensity is the safest and most effective approach.”
Other experts have emphasized the importance of tailoring exercise recommendations to individual needs and preferences. “There is no one-size-fits-all approach to exercise,” said Dr. Sarah Johnson, an exercise physiologist at the American Heart Association. “The best exercise program is one that you enjoy and can stick with over the long term.”
Dr. Johnson recommended that individuals consult with a healthcare professional or certified exercise specialist to develop a personalized exercise plan that is safe, effective, and enjoyable. “A qualified professional can help you to choose the right types of exercise, determine the appropriate intensity and duration, and monitor your progress,” she said.
Expanding the Scope: Types of Exercise and Blood Pressure
While the study focused primarily on exercise frequency, it’s important to consider the different types of exercise and their respective effects on blood pressure. Aerobic exercise, such as walking, running, cycling, and swimming, has been shown to be particularly effective at lowering blood pressure. Resistance training, such as weightlifting, can also contribute to blood pressure reduction, although its effects may be less pronounced than those of aerobic exercise.
A combination of aerobic and resistance training may be the most beneficial approach for overall cardiovascular health and blood pressure control. This type of program provides a well-rounded workout that targets different muscle groups and physiological systems.
It’s also important to note that even small amounts of physical activity can have a positive impact on blood pressure. Simple activities such as taking the stairs instead of the elevator, walking during lunch breaks, and gardening can all contribute to a healthier lifestyle and lower blood pressure.
The Role of Technology: Monitoring Exercise and Blood Pressure
Advances in technology have made it easier than ever to monitor exercise habits and blood pressure levels. Wearable fitness trackers can track steps, distance, heart rate, and other metrics, providing valuable insights into exercise activity. Home blood pressure monitors allow individuals to regularly check their blood pressure and track changes over time.
The data collected from these devices can be used to personalize exercise plans and monitor the effectiveness of lifestyle interventions. Individuals can work with their healthcare providers to interpret the data and make adjustments as needed.
However, it’s important to choose reputable and validated devices to ensure accurate measurements. It’s also crucial to understand the limitations of these technologies and to interpret the data in the context of overall health and well-being.
Looking Ahead: Future Research Directions
The study’s findings have opened up new avenues for research into the relationship between exercise and blood pressure. Future studies could explore the optimal combination of exercise frequency, intensity, and duration for hypertension management. Research could also investigate the effects of different types of exercise on blood pressure, taking into account individual characteristics such as age, sex, and health status.
Another important area of research is the role of genetics in determining individual responses to exercise. Some individuals may be more genetically predisposed to benefit from exercise than others. Understanding the genetic factors that influence exercise response could lead to more personalized exercise recommendations.
Finally, future studies could examine the long-term effects of exercise on blood pressure and cardiovascular health. This research could help to determine the optimal exercise strategies for preventing hypertension and reducing the risk of cardiovascular disease over the lifespan.
Conclusion: Embracing the Exercise Sweet Spot
The new study provides valuable insights into the optimal frequency of exercise for blood pressure control. Aiming for four to five days of physical activity per week appears to be the sweet spot for maximizing blood pressure reductions. However, it’s essential to remember that individual needs and circumstances vary, and personalized exercise plans should be developed in consultation with healthcare professionals.
By embracing the exercise sweet spot and incorporating regular physical activity into their daily lives, individuals can take control of their blood pressure and improve their overall cardiovascular health. Combined with other healthy lifestyle choices, exercise can be a powerful tool for preventing and managing hypertension and reducing the risk of heart disease and stroke.
Frequently Asked Questions (FAQ)
1. What is considered the “sweet spot” for exercise frequency to lower blood pressure, according to the study?
The study indicates that exercising four to five days per week is the “sweet spot” for maximizing blood pressure reductions. This frequency was found to be more effective than exercising less often or more often.
2. What types of exercise are most effective for lowering blood pressure?
While the study focused on exercise frequency, aerobic exercise (walking, running, cycling, swimming) is generally considered highly effective for lowering blood pressure. Resistance training can also contribute, and a combination of both types may be optimal.
3. Should I consult with a doctor before starting a new exercise program for blood pressure control?
Yes, especially if you have pre-existing health conditions like heart disease, diabetes, or kidney problems. A healthcare provider can assess your health status and provide guidance on safe and effective exercise strategies.
4. Does the intensity and duration of exercise matter, or is it just the frequency that impacts blood pressure?
While the study highlighted frequency, intensity and duration are also important. The study didn’t focus on this. General guidelines recommend moderate-intensity exercise for at least 30 minutes on most days of the week.
5. What other lifestyle changes can help lower blood pressure besides exercise?
Adopting a healthy diet (low in sodium, rich in fruits and vegetables), maintaining a healthy weight, limiting alcohol consumption, managing stress, and quitting smoking are all crucial lifestyle changes that can contribute to lower blood pressure.
Expanded Analysis: Beyond the Headlines
The Yahoo News report and the European Journal of Preventive Cardiology study it references bring to light an important refinement in our understanding of exercise and blood pressure management. While the universal recommendation is to engage in regular physical activity for overall health, the specific finding that four to five days of exercise per week may be optimal for blood pressure control is noteworthy. Let’s dissect the implications, potential limitations, and future directions emerging from this research.
The Importance of Exercise Frequency: A Nuanced Perspective
Previous guidelines often emphasized the duration and intensity of exercise, with frequency sometimes taking a back seat. This study places frequency squarely in the spotlight. Why might this be significant?
-
Consistency and Habit Formation: Exercising four to five times a week establishes a consistent routine. Regularity is a cornerstone of habit formation, making it more likely that individuals will adhere to an exercise program long-term. This sustained commitment is crucial for realizing the long-term benefits of exercise on blood pressure and overall cardiovascular health.
-
Physiological Adaptation: Consistent, moderately frequent exercise may allow the body to adapt more effectively to the physiological stress of physical activity. This adaptation involves improved blood vessel function, enhanced regulation of the nervous system, and optimized hormone balance, all of which contribute to blood pressure reduction.
-
Recovery and Repair: The study’s finding that exercising more than five days a week didn’t provide additional benefits and may have even been detrimental suggests the importance of adequate recovery. Rest days allow the body to repair muscle tissue, replenish energy stores, and adapt to the demands of exercise. Overdoing it without sufficient recovery could lead to fatigue, injury, and potentially, a blunted blood pressure response.
Limitations and Caveats: A Critical Appraisal
While the study’s findings are compelling, it’s essential to acknowledge its limitations and consider these caveats when interpreting the results:
-
Meta-Analysis Design: The study was a meta-analysis, meaning it synthesized data from previously published studies. Meta-analyses are powerful tools, but they are limited by the quality and consistency of the original studies. Variations in study design, participant characteristics, and exercise protocols could introduce bias and affect the overall results.
-
Lack of Specificity: The study didn’t specify the ideal intensity or duration of each exercise session. This leaves room for interpretation and makes it challenging to translate the findings into precise exercise recommendations. Future research is needed to clarify the optimal combination of frequency, intensity, and duration.
-
Observational Nature: Many of the original studies were observational, meaning they observed the relationship between exercise habits and blood pressure without directly manipulating exercise interventions. Observational studies can identify associations, but they cannot prove cause and effect. It’s possible that other factors, such as diet or stress levels, could explain the observed association between exercise frequency and blood pressure.
-
Individual Variability: The study’s findings represent a population-level average. Individual responses to exercise can vary widely based on factors such as age, genetics, health status, and fitness level. What works for one person may not work for another.
-
Self-Reported Data: Some of the original studies relied on self-reported exercise data, which can be subject to recall bias and inaccuracies. Individuals may overestimate or underestimate their exercise activity, leading to errors in the analysis.
Future Research Directions: Filling the Gaps
The study highlights several key areas for future research:
-
Randomized Controlled Trials: Randomized controlled trials (RCTs) are needed to confirm the causal relationship between exercise frequency and blood pressure. RCTs involve randomly assigning participants to different exercise groups and directly manipulating exercise interventions. This type of study design provides stronger evidence of cause and effect.
-
Dose-Response Relationships: Future studies should investigate the dose-response relationship between exercise frequency, intensity, duration, and blood pressure. This would involve examining how different combinations of these exercise variables affect blood pressure outcomes.
-
Mechanistic Studies: Research is needed to elucidate the mechanisms by which exercise frequency affects blood pressure. This could involve studying the effects of exercise on blood vessel function, nervous system activity, hormone levels, and other physiological parameters.
-
Personalized Exercise Prescriptions: Future research should focus on developing personalized exercise prescriptions that take into account individual characteristics and preferences. This could involve using genetic testing, biomarkers, and wearable technology to tailor exercise recommendations to each individual’s unique needs.
-
Long-Term Outcomes: Studies are needed to examine the long-term effects of exercise frequency on blood pressure and cardiovascular health. This would involve following participants over many years to assess the impact of different exercise patterns on the risk of heart disease, stroke, and other adverse outcomes.
Practical Applications: Translating Research into Action
Despite the limitations, the study’s findings offer valuable guidance for individuals seeking to manage their blood pressure through exercise:
-
Aim for Four to Five Days: Strive to engage in physical activity four to five days per week. This frequency appears to be optimal for blood pressure control.
-
Mix It Up: Incorporate a variety of exercise types into your routine. Aerobic exercise, resistance training, and flexibility exercises all offer different benefits.
-
Listen to Your Body: Pay attention to your body’s signals and avoid overtraining. Allow for adequate rest and recovery between workouts.
-
Start Slowly: If you’re new to exercise, start gradually and gradually increase the frequency, intensity, and duration of your workouts.
-
Consult a Professional: If you have pre-existing health conditions or are unsure about how to start an exercise program, consult with a healthcare provider or certified exercise specialist.
-
Make It Enjoyable: Choose activities that you enjoy and are likely to stick with over the long term. Exercise should be a sustainable part of your lifestyle.
-
Track Your Progress: Use a fitness tracker or blood pressure monitor to track your progress and stay motivated. Seeing tangible results can help you stay on track.
The Broader Context: Exercise as a Cornerstone of Cardiovascular Health
It’s important to remember that exercise is just one component of a comprehensive approach to managing blood pressure and promoting cardiovascular health. Other essential lifestyle modifications include:
-
Healthy Diet: Adopt a heart-healthy diet that is low in sodium, saturated fat, and cholesterol, and rich in fruits, vegetables, and whole grains. The DASH (Dietary Approaches to Stop Hypertension) diet is a well-established eating plan for lowering blood pressure.
-
Weight Management: Maintain a healthy weight. Obesity is a major risk factor for hypertension and other cardiovascular diseases.
-
Stress Management: Practice stress-reducing techniques such as yoga, meditation, or deep breathing exercises. Chronic stress can elevate blood pressure.
-
Smoking Cessation: Quit smoking. Smoking damages blood vessels and increases the risk of cardiovascular disease.
-
Medications: In some cases, medication may be necessary to achieve adequate blood pressure control. If your doctor prescribes medication, take it as directed and follow their recommendations.
Conclusion: A Call to Action
The new study underscores the importance of exercise for blood pressure management and provides valuable insights into the optimal frequency of physical activity. By aiming for four to five days of exercise per week, individuals can potentially maximize the blood pressure-lowering benefits of exercise. However, it’s crucial to remember that individual needs vary, and personalized exercise plans should be developed in consultation with healthcare professionals.
By embracing a holistic approach that combines regular exercise with other healthy lifestyle choices, individuals can take control of their blood pressure and significantly reduce their risk of cardiovascular disease. This is not just about living longer; it’s about living healthier and enjoying a higher quality of life.









